This event is called a Healing Story Session, but technically, my story begins with health, not illness. As a prospective kidney donor, the whole point was for me to be as healthy as possible, and I was. But there was something wrong with me that day in January 2018, when I scrolled through Facebook to find my friend and colleague Mike Romano telling us that, having been diagnosed with polycystic kidney disease, he now found himself asking the “difficult” question: was there anyone in his orbit who would be willing to consider donating a kidney to him? What felt difficult to him to ask felt immediately, unquestionably, and profoundly right to me to answer in the affirmative. Because despite having general good health, the right blood type, and two kidneys that had always seemed to function quite well, I did have an affliction that weighed upon me. I believe that my subconscious soul recognized in this kidney journey the possibility of beginning to heal my heart, which had broken just two months before, on November 5, 2017, when I found my mother dead on the floor of her house. In the shock and emptiness I had felt since that day, I nevertheless spied something in the possibility of organ donation that might fill me again with peace.
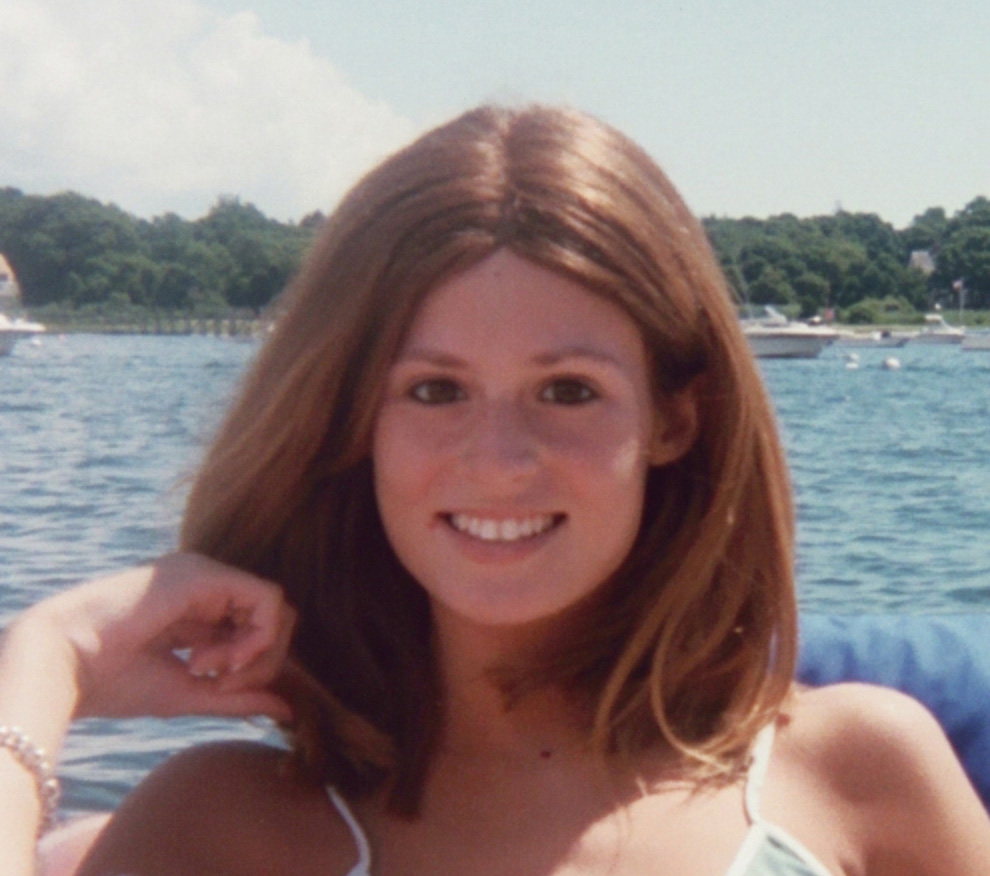
My mother, Yvonne, was diagnosed with cancer in her tonsils in late October of 2016, at age 79, just four months after the death of her husband of nearly 30 years, my stepfather Jim. The year between her diagnosis and her death featured the full array of treatments at the Dana-Farber Cancer Institute, including both chemotherapy and radiation. Because of the intensity of the course of treatment, she spent several weeks on the cancer floor at the Brigham and Women’s Hospital, as well as extended stays at three different rehab facilities. The the treatment period was seven weeks, but because of the severity of its effects, Yvonne was continuously hospitalized or in rehab for more than three months. My brother Henry and I, her only children, spent much of our time with her, at appointments and treatment sessions, in hospitals and nursing homes, so that she wouldn’t be alone. I was stunned when I joined her for a chemo session for the first time, as the nurse who was administering the drug arrived wrapped in double layers of gowns to protect herself from even touching the very substance that was about to be dripped into my mother’s veins. On another day at the Brigham, a nurse saved her life in what seemed to me to be a major heart event that had nothing to do with the cancer but everything to do with the unendurable pain of her burned-out throat. Even in May, when the oncologist declared her cured of the cancer, she was still stripped her of her ability to eat and the feeding tube that had been installed months before had to remain in place, as she slowly retrained herself to consume food, even when it tasted wrong and metallic and miserable.
Growing up in Brookline, Mass., my mother having worked as an administrator at Harvard Medical School and the Brigham for years, it was an article of faith that we were so lucky to live in this part of the country. It was like a talisman, I now see - one of the charms of what I think I thought of as my charmed life. Not perfect, not without sadness or failure or misfortune - but happy underneath it all. The day in November 2016 when Henry and I joined our mother on the Head & Neck floor of the Farber, when Dr. Rabinowitz told her that they had found cancer on her tonsils and adjacent lymph nodes, it was bad. But we were in the place that people came to from everywhere in the world to be treated for these things; this was a place with an entire floor devoted to precisely the kind of cancer my mother had. In the way that the radiation team targeted her cancer within millimeters with their fierce rays, that’s how focused these people were on specific types of cancer. What I would learn, of course, is that no matter how targeted the radiation, the physical pain would spread just as malignantly as the disease that was being stopped. In fact, it was the very way that they were focused, each in their own way, that precluded them from being able to see Yvonne as she was, fragile and stoic and terrified and alone in a fundamental way for the first time in more than 30 years. The way different people kept asking the same questions about where she lived and with whom and whether she was married made it clear that no one saw her that way except for Henry and me, and our spouses. That seemed wrong, in a way I couldn’t exactly identify, but that I felt in my heart.
The events of February 3, 2017 captured this dissonance for me perfectly. It was the last day of eight weeks of 5 days/week of radiation, and at this point she was inpatient at the Brigham’s “Cancer Center for Excellence.” I had left work early to meet her there and spend some time with her afterwards, and when I arrived, I found her very confused about what was happening to her; not the first time I had encountered her in this state, either a result of the overwhelming pain she was in or as part of the side effects of a Fentanyl patch for that pain. She was in tears and wanted me to go into the treatment room with her - not permitted. Eventually, we were able to reassure her that it was OK and no one was going to hurt her (?!), and she proceeded to the lab. When she came out, one of the two nurses who had followed her case came to say goodbye and asked us to wait a minute before returning to the Brigham. She returned shortly with a bubble gun to fill the area with bubbles in a celebration of the end of the course of radiation. She couldn’t have been kinder or had better intentions, and I even took pictures of the three of us; but all I see when I look at it now is a film of smiles over the ocean of my mother’s agony, and a kind of willful misunderstanding of that moment in a cancer patient’s course of treatment. It got so much worse after that point - they had told us that it would, as the effects of the chemicals and burning reverberated through my mother’s frail body - but that bubble gun “celebration” belied any real grasp of what that would mean for her and for us.
So all of this time in medical and medicine-adjacent places left me confused about what the words “treatment” and “cure” and “healing” meant. And even while I was grateful to have these purported world-class facilities available to her, I couldn’t help question, as the months went on, whether any of the dozens of people who interacted with her really cared about her in the way that would lead her back to authentic good health. Just like the nurse in radiation, everyone we met, individually, was kind and smart and knew their stuff, but each was only treating an aspect of her illness; and it was all so big and terrifying that I could never find the right way to ask the right question of the right person. I just wanted her to be OK, and when by July she was finally home, living on her own again, I felt like I could breathe and let those questions go. Then I arrived at her house on that November Sunday and found her dead, all those questions ballooned into shrieks of pain and confusion and heartbreak that haunt me still. We’ll never know what happened to her, though we suspect an internal bleed following the removal of the feeding tube. Maybe her heart gave out, maybe there were other sequelae to her treatment. All I know is that this was my malady: not just the personal, crushing loss of a mother who offered unconditional love for all of the 54 years we had together, but also the faltering of my belief in these medical practices and practitioners and institutions.
This was my frame of mind when I saw Mike’s post about his need for a kidney. In the moment, I only really registered two things: I had the correct blood type (O+), and I like to fill out forms. So I hopped on the MGH screening site and filled to my heart’s content. I honestly never thought I’d be chosen as a kidney donor; I thought for sure my age would knock me out, or my somewhat overweightness, or a million other things - it seems deeply out-of-this-world to contemplate being an organ donor. Mike and I have known each other for more than ten years, since he joined me at Acton-Boxborough Regional High School - him teaching science, me English. Our fields are different - “opposites” in a lot of the ways that many schools operate. But we have had many students in common and I have learned from them of his gifts for inspiring a love of science, its processes and discoveries and possibilities. We have co-advised the school’s Student Council and chaperoned proms together. We have served together on union boards, where my urge to placate has balanced against his willingness to engage in the fight. Early in his career, we were two of the final three competitors in a student-run spelling bee and I was crushed when his deep knowledge of fancy Latinate science words took me out. I am in awe for his many gifts, of language and communication in addition to his enthusiasm and curiosity in his chosen field, and I can say now that I’ve always felt a kind of big-sister affection for him.
I will never forget getting the email, just before February vacation in 2018, saying I was a potential match. I was sitting at my desk in my classroom, and it actually did feel like being struck by lightning. I had a sense of being suddenly lifted above of my misery, deposited in a place where death and my grief could recede and the possibilities of life were manifest. After feeling frustrated and sidelined during my mother’s treatment and ultimately mystified by her death, it seemed suddenly possible that I could move to the center of a life-saving story. I called Mike right away in Washington, where he was spending a sabbatical year as an Einstein Fellow working at NASA. It never occurred to me not to tell him that I was a possible match, in case I might have wanted to change my mind, because I knew, without knowing why, that there was never a question of changing my mind. I was a little bit giddy when I called to let him know that I was a “green light” candidate, meaning that I would be scheduled for the proverbial battery of tests before learning whether I could actually donate or not. I think we were both stunned that after a literal worldwide response to his initial post, his potential donor could be just down the hall in the west wing of the high school. He assured me that his need for a new kidney was urgent in the “within 6-8 months” sense, and not the “next week during February vacation” sense, and I relaxed, for a while.
Every step of the testing held an odd kind of thrill for me. I can now see that the whole process was a mirror image of my experience with my mother, which certainly contributed to that feeling. Because the donor has their own team of professionals, separate from the recipient’s team, I was the focus of attention of a group of people dedicated to one goal: making sure I was fit for a major surgery and its aftermath. In a way, they had the same intensity of focus as the oncologists and radiologists who had treated my mother, but the expertise of each member of the team seemed to me to be integrated instead of exclusive. I met with my nurse, Kelly, and my social worker, Judy, and each of them took great pains and time to make sure I knew what to expect, and to learn about me and my story. Even parts of my life outside the Mass. General were folded into the process: when I met with the psychiatrist on the team, and I told him that I was talking with my own therapist about the possibility of transplant, he asked if I would allow him to speak with her. I agreed, and even felt buoyed by the idea that he was taking such care. I did a series of respiratory tests to determine my lung capacity because I smoked for 18 years - though I quit nearly 20 years ago. It felt as though I started the process feeling mildly good about my own health and by the time I got to surgery on October 25, I felt like a superwoman.
I should talk here about what passed between me and Mike in all this time. The testing began in March of 2018, and proceeded through the end of June. I checked in with Mike periodically, though we were both incredibly busy and several states apart at the time. And as I’ve said, we aren’t friends, as such - we don’t hang out, we don’t socialize. We’re close as colleagues, but if I eventually gave him my kidney, it would not be because of our deep personal bond. I think it was something that confused some people when I first started talking about the possibility of organ donation. When I said that the possible recipient wasn’t a relative or close friend, I felt mystification and even concern start to emanate. I couldn’t really explain it myself, this bubbling elation I felt whenever I imagined my nurse Kelly telling me that we were a “go” for donation. I just knew that I didn’t want to let it go.
My social worker Judy raised this question, in reverse, during the testing period. We talked about how I would feel if I got a “no” from Kelly, and what I would do to manage that feeling; how I would even prepare for the call itself, when it came, regardless of the verdict. I told her I would be devastated if I couldn’t donate, though in truth, this felt like it was more about me than about Michael. I had seen the Facebook response, I knew how much he meant to so many people. I couldn’t imagine that another donor couldn’t be found. When I examined this potential “no,” I simply felt as if something would be taken from me - ironic, since that “no” would actually mean I would get to keep something, a kidney. I couldn’t explain it, and I just hoped I didn’t sound too zealous to be a good donor. We also agreed that if I saw Kelly’s name on an incoming call, I should sit down to take it.
And then, there it was: Kelly called me in June, after the kidney team had met, just as she said she would. I took a seat, as I had promised Judy I would. And as you know, it was a “yes.” The relief, the elation, the surrealness, they all exploded in me. Kelly asked if I wanted to be the one to tell Mike, and to be able to do that felt like another gift. We agreed that Mike and I would start to think about potential surgery dates, after she said what felt like the weirdest thing: “We usually do these transplant surgeries on Tuesdays and Thursdays, so keep that in mind when picking dates.” The bigness of my feelings compared with the everydayness of that statement still makes me laugh. I texted Mike to see if he was free, and asked him to call me if he was. I don’t remember the exact words that passed between us, but it was a very good vibe on that line from Needham to Washington DC. We didn’t talk long, in the end, past deciding that we would start looking at dates (Tuesdays & Thursdays!) as he wrapped up at NASA and I proceeded into summer travels.
I knew that Mike would be busy wrapping up his year in DC and moving back to Cambridge in late July/early August. I also knew that this surgery, and its aftermath, were probably much heavier for him to contemplate than they were for me. I was desperate for my kidney to work for him, but even if it didn’t, I would come out of the surgery relatively unscathed. He had many more reasons to hesitate, while I felt nothing but full-steam-ahead. As August ticked along and we hadn’t picked a date yet, I started to worry that he might not want to go through with it, or that he might prefer a donation from a stranger rather than being tied to me in this way for the rest of his life. Finally, on August 27, I wrote Mike an email, which included the following: “The only other thing is to tell you how profoundly happy this process makes me - and how incredibly lucky I feel to be able to do this with you. I don't know if that sounds ridiculously saccharine and hard to believe, but I swear to you it's the whole, unmitigated truth. It makes me happy to think I'll have a connection to you in this way, but I don't want you to think that possession of one of my kidneys will lead to any possessive stalking on my part; once it's yours, it's all yours, and if you want to take it around the world on a binge when you turn 40, have at it!” I read this now, and the intensity of how much I wanted this to work suffuses me again. I literally could not wait to give something of myself, of my own body, and I felt lucky at the prospect of an entirely voluntary, deeply invasive surgical procedure. I couldn’t explain it then any better than I did - “take my kidney for a joyride!” - but as I’m writing this piece, it’s starting to come into greater focus. Mike didn’t reply to that email, and he didn’t have to; it was enough that I had made my intentions clear. Soon after, we texted some possibilities back and forth - as we like to say, “like you’d schedule a coffee date” - and eventually settled on Thursday, October 25.
When that day came, I felt not one instant of pain or fear, but instead a kind of stillness and peace. From my bed in the pre-op unit, I could see the electronic board listing various surgeries; in the medical shows on TV, it’s a messy whiteboard, but this was a beautifully intelligent screen. I realized that all the surgeries were inching to the left along a timeline. Even without my distance glasses, I could just make out “kidney transplant” on the board, and I zeroed in on that entry until it met its destination time of 10 a.m. I also remember thinking, it’s a good thing I started taking anti-anxiety medication 20 years ago, in preparation for this very moment, which back then would have been suffused with dread, instead of the peaceful anticipation of today. If I leave you with anything today, let it be an endorsement for good mental health care. Our surgeries having crossed the timeline, it was time to go; I was wheeled to the very, very bright operating room, told that the mask would smell like a beach ball, start to count backwards, and I’m out.
But two seconds later, I’m back. If you’ve never had surgery - as I never had - you should be aware that it’s not like sleeping. There are no dreams, there’s no sense of any time passing at all. It seems quite inconceivable that anything could have happened in the few seconds you were out. But of course, it wasn’t seconds, it was hours, at least four hours, and someone is pushing their knuckles into my chest to wake me up, and all I remember saying as I opened my eyes was, “Did it work? Is it working?” I needed to know if my kidney was functioning inside Mike, and they told me right away that it was. Hallelujah! I had no more words, but I was happy to be rolled to a room on the same floor where Mike would eventually also arrive, though his surgery would take longer than mine.
People want to know about everything I had to “go through,” the restrictions I must have had, or still have, on what I eat or drink, on whether I feel different being down a kidney. But the truth is, from the very first hours of recovery, it’s just not that big a deal. This might have been influenced by the fact that my roommate for most of my two night stay at the Mass. General was a heart transplant recipient with multiple woes, so my situation truly paled in comparison. I was uncomfortable, to be sure - the particulars of expelling the gas used to inflate my belly so that Dr. Dageforde could reach in with her exquisitely small hands through the incision around my belly button to extract my left kidney - I’ll leave them to your imagination. I couldn’t roll onto either side, and lying on your back is a drag after a while. But nothing about my diet has changed, nothing about the way my body functions has changed, and there was never a moment from when I was awoken that I wasn’t in awe, in relief, in joy. My husband Dan, no fan of hospitals, stayed with me, and my brother Henry and sister-in-law Mimi arrived from the waiting area where it turned out that they had met and bonded with Karen and Angelo, Mike’s parents. It was, in the most elemental and profound way, all good.
And here we are now, almost exactly seven months to the day from that day. Whenever someone comments on what I did, the only thing I can ever say is how lucky I feel to have been able to do it. I’ve said it reflexively and for a long time I thought it was because I got to be the person who makes such a difference in the life of another person. But in telling this story, I’ve been pushed to unpack what I really meant by that, at first just to myself and now to all of you. And of course, you’ve probably guessed by now what it turns out I meant: the luckiest thing about this adventure was that it came at the exact moment when I needed to be rescued from the very worst reality by the very best possibility. I needed to be able to focus on my body and what it was capable of so that I could get out of my head and even my heart and the sadness by which both were bound. Being one of about 65 living donors in 2018 at the Mass. General was the opposite in every way of being one of thousands of patients at the Dana Farber, which was Yvonne’s plight. In a conversation with Annie Brewster, when I was wrestling with this story, she drew my attention to something that’s a little bit raw, but I can’t get the image out of my head: I have told you that we think that the removal of Yvonne’s feeding tube might have contributed to her death. It’s a common enough procedure, the tube being yanked out a little abruptly - as she described it to us that night - and almost never dangerous. And yet there she was, the next day, dead on the floor. I told this to Annie, and after a pause, she pointed out that I also had something removed from my body - but with care, and thought, and intention. And not only am I still here to tell the story, but much, much more importantly, so is Michael.